What is it?
Vaginal cancer is a rare cancer that occurs in your vagina — the muscular tube that connects your uterus with your outer genitals. Vaginal cancer most commonly occurs in the cells that line the surface of your vagina, which is sometimes called the birth canal.
While several cancers can spread to your vagina from other places in your body, cancer that begins in your vagina (primary vaginal cancer) is rare. Vaginal cancer comprises only 2 to 3 percent of gynecologic cancers.
Women with early-stage vaginal cancer have the best chance for a cure. Vaginal cancer that spreads beyond the vagina is much more difficult to treat.
Symptoms
Early vaginal cancer may not have any signs and symptoms. As it progresses, vaginal cancer may cause signs and symptoms such as:
- Unusual vaginal bleeding, such as after intercourse or after menopause
- Watery vaginal discharge that may be bloody and foul smelling
- Lump or mass in your vagina
- Painful urination
- Constipation
- Pelvic pain
Causes
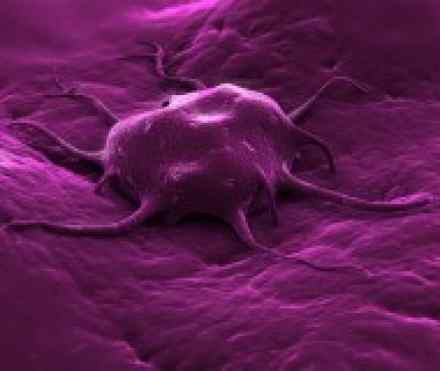
In general, cancer begins when healthy cells acquire a genetic mutation that turns normal cells into abnormal cells. Healthy cells grow and multiply at a set rate, eventually dying at a set time. Cancer cells grow and multiply out of control, and they don't die. The accumulating abnormal cells form a mass (tumour). Cancer cells invade nearby tissues and can break off from an initial tumor to spread elsewhere in the body (metastasize).
The majority — 85 to 90 percent — of vaginal cancers begin in the squamous cells. These thin, flat cells line the surface of your vagina. Other less common types of vaginal cancer include:
- Vaginal adenocarcinoma, which begins in the glandular cells on the surface of your vagina
- Vaginal melanoma, which develops in the pigment-producing cells (melanocytes) of your vagina
- Vaginal sarcoma, which develops in the connective tissue cells or smooth muscles cells in the walls of your vagina
As is the case with many types of cancer, it isn't clear what causes the genetic mutation that leads to vaginal cancer.
Risk factors
Certain factors may raise your risk of vaginal cancer, though women with no known risk factors can also develop vaginal cancer. Risk factors for vaginal cancer include:
- Age. Most women who are diagnosed with vaginal cancer are over 60 years old.
- Atypical cells in the vagina. Women with vaginal intraepithelial neoplasia (VAIN) have an increased risk of vaginal cancer. In women with VAIN, cells in the vagina appear different from normal cells, but not different enough to be considered cancer. A small number of women with VAIN will eventually develop vaginal cancer, though doctors aren't sure what causes some cases to develop into cancer and others to remain benign.
- Exposure to miscarriage prevention drug. Women whose mothers took a drug called diethylstilbestrol (DES) while pregnant have an increased risk of a certain type of vaginal cancer called clear cell adenocarcinoma. DES was used from the late 1940s until 1971 to prevent miscarriage in early pregnancy.
- Human papillomavirus (HPV). HPV is a sexually transmitted virus that can increase the risk of vaginal cancer and other cancers. HPV causes the majority of cervical cancers and precancerous changes in the cervix. A vaccine (Gardasil) that prevents some types of HPV is available.
- Previous gynecologic cancer. Women who've been treated for a different gynecologic cancer, especially cervical cancer, may have an increased risk of vaginal cancer.
Other risk factors that have been linked to an increased risk of vaginal cancer include:
- Multiple sexual partners
- Early age at first intercourse
- Smoking
- HIV infection
Complications
Vaginal cancer may spread (metastasize) to distant areas of your body, such as your lungs, liver and pelvic bones.
Diagnosis
While there is no general screening test for vaginal cancer, it's sometimes found during a routine pelvic exam before signs and symptoms become evident. During a pelvic exam, your doctor carefully inspects the outer exposed part of your vagina, and then inserts two fingers of one hand into your vagina and simultaneously presses the other hand on your abdomen to feel your uterus and ovaries. He or she also inserts a device called a speculum into your vagina. The speculum widens your vagina so that your doctor can check your vagina and cervix for abnormalities.
Your doctor usually also conducts a Pap test to screen for cervical cancer, but sometimes vaginal cancer cells can be detected on a Pap test. Pap tests and pelvic exams are generally recommended every two to three years. How often you undergo these screenings depends on your risk factors for cancer and whether you've had abnormal Pap tests in the past. Talk to your doctor about how often you should have this health screening.
If you have any signs and symptoms, your doctor may conduct a pelvic exam and Pap test to check for abnormalities that may indicate vaginal cancer. Additionally, your doctor may conduct other procedures to determine whether you have vaginal cancer, such as:
- Colposcopy. Colposcopy is an examination of your vagina with a special lighted microscope called a colposcope. Colposcopy allows your doctor to magnify the surface of your vagina to see any areas of abnormal cells.
- Biopsy. Biopsy is a procedure to remove a sample of suspicious tissue to test for cancer cells. Your doctor may take a biopsy of tissue during a colposcopy exam. Your doctor sends the tissue sample to a laboratory for testing.
Staging
Once your doctor diagnoses vaginal cancer, he or she takes steps to determine the extent of the cancer — a process called staging. The stage of your cancer helps your doctor decide what treatments are appropriate for you. In order to determine the stage of your cancer, your doctor may use:
- Biopsy. Tissue samples from your cervix or vulva may show whether cancer has spread to those areas.
- Imaging tests. Your doctor may order imaging tests to determine whether cancer has spread. Imaging tests may include X-rays, computerized tomography (CT) scans or magnetic resonance imaging (MRI).
- Tiny cameras to see inside your body. Procedures that use tiny cameras to see inside your body may help your doctor determine if cancer has spread to certain areas. Cameras help your doctor see inside your bladder (cystoscopy) and your rectum (proctoscopy).
- Positron emission tomography (PET) scan. This test uses sugar (glucose) combined with a radioactive atom to detect areas where cancer has spread. Cancer cells use more glucose because they're more active than normal cells, and the PET scan highlights areas where it isn't always easy to noninvasively detect cancer, such as your lymph nodes.
Once your doctor determines the extent of your cancer, he or she assigns your cancer a stage. The stages of vaginal cancer are:
- Stage 0. Cancer hasn't spread past the first layer (epithelium) of the vaginal wall. Five-year survival rates at this stage are as high as 96 percent.
- Stage I. Cancer is limited to the vaginal wall.
- Stage II. Cancer has spread to tissue next to your vagina.
- Stage III. Cancer has spread to nearby lymph nodes, or to the pelvic wall or both.
- Stage IVA. Cancer has spread to nearby lymph nodes, and has also spread to your bladder, rectum or pelvis.
- Stage IVB. Cancer has spread to areas away from your vagina, such as your lungs.
References
http://www.medicinenet.com/vaginal_cancer/article.htm
http://www.webmd.com/cancer/tc/vaginal-cancer-treatment-patient-information-nci-pdq-general-information-about-vaginal-cancer
http://www.nhs.uk/Conditions/Cancer-of-the-vagina/Pages/Introduction.aspx
https://www.hse.ie/eng/health/az/C/Cancer,-cervical/Causes-of-cervical-cancer.html

