What is it?
- Vascular dementia is an umbrella term that describes impairments in cognitive function caused by problems in blood vessels that feed the brain.
- In some cases, a blood vessel may be completely blocked, causing a stroke. Not all strokes cause vascular dementia. It depends on the severity of the stroke, where the stroke occurred and the portion of the brain that's affected.
Symptoms
Vascular dementia symptoms can vary, depending on the portion of the brain that's affected. People with vascular dementia can experience:
- Confusion and agitation
- Problems with memory
- Unsteady gait
- Urinary frequency, urgency or incontinence
- Night wandering
- Depression
- A decline in the ability to organize thoughts or actions
- Difficulty planning ahead
- Trouble communicating details sequentially
- Memory loss
- Poor attention and concentration
Vascular dementia symptoms often begin suddenly and may worsen in a stepwise fashion, following a series of strokes or ministrokes. But some forms of vascular dementia develop gradually and can easily be confused with Alzheimer's disease.
Adding to the confusion, Alzheimer's disease and vascular dementia often occur together. In fact, some scientists believe that it's more common for these two disorders to occur together than apart.
Causes
Vascular dementia is most often caused by either a:
- Complete blockage of blood vessels in the brain. The complete blockage of an artery in the brain usually causes a stroke (infarction), but some blockages don't produce stroke symptoms. These "silent brain infarctions" increase a person's risk of vascular dementia. The risk increases with the number of infarctions experienced over time. One variety of vascular dementia is called multi-infarct dementia. Heart disease and irregular heart rhythms, such as atrial fibrillation, can increase your risk of stroke.
- Narrowing of the blood vessels in the brain. Vascular dementia also can occur without a complete blockage of an artery. Portions of the brain can be starved for oxygen and food by reduced blood flow from arteries narrowed by vascular disease.
Vascular dementia can also be caused by:
- Profoundly low blood pressure
- Brain damage caused by brain hemorrhage
- Blood vessel damage from such disorders as lupus erythematosus or temporal arteritis
Risk factors
Risk factors for vascular dementia include:
- Increasing age. This is one of the biggest risk factors for vascular dementia. The disorder is rare before the age of 65. And people in their 80s and 90s are much more likely to have vascular dementia than people in their 60s and 70s.
- History of stroke. The brain damage that occurs with strokes appears to increase the risk of developing dementia.
- Hardening of the arteries (atherosclerosis). Atherosclerosis occurs when plaque builds up in your arteries and narrows your blood vessels. This can increase your risk of vascular dementia.
- High blood pressure. Hypertension puts extra pressure on blood vessels throughout the body. This increases the risk of vascular problems in the brain.
- Diabetes. High glucose levels damage blood vessels throughout the body, increasing the risk of stroke and other vascular problems in the brain.
- Smoking. Smoking increases the risk of hardening of the arteries and other vascular diseases, including vascular dementia.
- High cholesterol. High levels of bad cholesterol (LDL) are associated with an increased risk of vascular dementia, and possibly with a higher risk of Alzheimer's disease.
Diagnosis
If vascular dementia is suspected, your doctor may recommend one or more of the following tests:
- Computerized tomography (CT). A CT scan uses special X-ray equipment to produce a cross-sectional image showing a slice of your body's organs and tissues. A contrast material may be injected to help highlight any abnormalities in your brain's blood vessels.
- Magnetic resonance imaging (MRI). An MRI scan uses radio waves and a strong magnetic field to produce detailed images of internal organs and tissues. In some cases, contrast material may be injected to produce even more detailed pictures. Some people experience a feeling similar to claustrophobia when they're inside an MRI machine. If you think this will be a problem, your doctor can prescribe medication to help you relax.
- Positron emission tomography (PET). During a PET scan, you'll be injected with a low-level radioactive material, which binds to chemicals that travel to the brain. You lie on a table while an overhead scanner tracks the radioactive material. This helps show which parts of your brain aren't functioning properly. The test is painless and can be particularly useful in distinguishing between different types of dementia.
- Doppler ultrasound. Doppler ultrasound uses high-frequency sound waves to measure the direction and speed of blood cells as they travel through blood vessels — such as the carotid arteries, which travel through either side of your neck to connect your heart and brain. A Doppler ultrasound of your carotid arteries can help your doctor determine if there are blockages or narrow places impeding blood flow to your brain.
- Neuropsychological tests. Neuropsychological tests assess orientation, learning, recall, attention, calculation and language. Exam results for people with vascular dementia typically show the same types of cognitive deficits as the exam results of people who have Alzheimer's disease. One major difference, however, is in memory function. Most people with vascular dementia don't experience memory problems until later in the course of the disease unless there is a stroke in the exact area of the brain that controls memory.
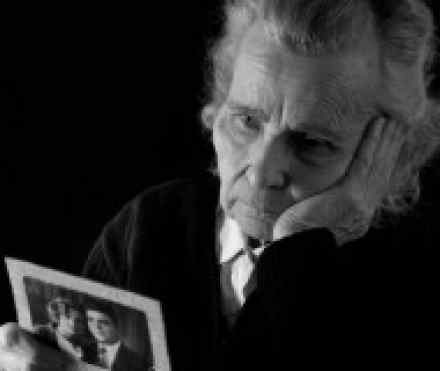
Living with vascular dementia
A diagnosis of dementia is scary. But it’s important to remember that many people with dementia lead healthy, fulfilling lives for years after the diagnosis. Don’t give up on life! As much as possible, continue to look after your physical and emotional health, do the things you love to do, and spend time with family and friends.
- Stay active as much as possible. Research suggests that even a leisurely 30-minute walk a day may reduce the risk of vascular dementia and help slow its progression. It will also boost your overall health and happiness.
- Create a network of support. Seeking help and encouragement from friends, family, health care experts, and support groups can improve your outlook and your health.
- Eat for heart health. Heart disease and stroke share many of the same risk factors, such as high LDL cholesterol (bad cholesterol), low HDL cholesterol (good cholesterol), and high blood pressure. Adopting a more heart-healthy diet may improve or slow down your dementia symptoms.
- Make it a point to have more fun. Laughing, playing and enjoying yourself are great ways to reduce stress and worry. Joy energizes and inspires lifestyle changes that prevent further strokes and blockages and compensate for memory and cognitive losses.
- Learn how to relax and manage stress. Stress is a major contributor to high blood pressure and heart disease, so it’s helpful to practice relaxation techniques, such as yoga, meditation, deep breathing, or rhythmic exercise, and know how to quickly reduce stress in the moment by employing one or more of your senses.
- Challenge your brain. Your brain remains capable of change throughout your life, so you may be able to improve your ability to retain and retrieve memories. Set aside some time in the evening to recall the day’s events, which can build memory capacity. Learning new skills, such as a foreign language or how to paint, can also help build brain capacity if done consistently.
Helping someone with vascular dementia
Caring for a person with vascular dementia can be very stressful for both you and your loved one. You can make the situation easier by providing a stable and supportive environment.
A stable environment starts with a stable, healthy you. It’s easy to lose sight of your own needs when your loved one is dealing with dementia. But taking care of yourself isn’t optional. Stress and burnout are common in caregivers—and that isn’t a good thing for you or the person you’re caring for. Nurturing and protecting your own emotional and physical health isn’t selfish. It’s the best thing you can do for the person you love.
Tips for caring for a loved one with vascular dementia
- Avoid changing things up. Your loved one will feel more comfortable and less frightened or agitated when he or she is on a regular routine and in familiar surroundings.
- Use calendars and clocks. Place large calendars and clocks around your loved one’s living area. They can help people with dementia reorient if they've forgotten the date or time.
- Keep your loved one busy. Encourage your loved one to continue physical and social activities as long as possible. Whether it’s going for a walk or spending time at the local senior center, it’s important that he or she has regular activities to participate in.
- Provide plenty of stimulation. Make sure your loved one’s room is colorful and inviting. Do they have a nice view outside? If not, you can bring the outdoors in with some flowers or a plant. Also make sure they have a TV, radio, or other things to look at and do.
-
Tell your loved one what you’re doing, and why. If it’s time for dinner, say so. Don’t just lead them into the kitchen without explaining what’s going on. Be sure to communicate, even if you’re not sure your loved one understands. Even if he or she doesn’t understand your words, your tone of voice and body language can provide reassurance.
References:
http://www.alz.org/dementia/vascular-dementia-symptoms.asp
https://www.alzheimers.org.uk/site/scripts/documents_info.php?documentID=161
http://en.wikipedia.org/wiki/Multi-infarct_dementia
http://www.helpguide.org/elder/vascular_dementia.htm
http://www.mayoclinic.com/health/vascular-dementia/DS00934
http://www.nhs.uk/Conditions/vascular-dementia/Pages/Introduction.aspx

